ELIMINATING PRE-ANALYTICAL ERRORS
A PAMS foundation stone.
Taking a new approach to an ever growing problem for labs world-wide.
THE CHANGING LABORATORY LANDSCAPE
Diagnostic testing is becoming an ever more important diagnostic tool for healthcare as it seeks more efficient and effective methods to improve the quality of healthcare services. Internationally, in 2015, labs processed in excess of 10 billion diagnostic tests. Around 70% of all medical decisions are now influenced by the results of diagnostic testing. Even with an error rate of 0.1% this equates to over 10 million errors every year – and we know that 0.1% is at the lower end of the real error rate. Of all of these errors, most are now due to errors originating in the Pre-Analytical process.
The range and sophistication of laboratory tests available has dramatically increased and with it the demands on laboratories and clinicians to ensure error free delivery of laboratory test results. As clinicians rely more heavily on laboratory testing to confirm the diagnosis of patient conditions and to determine the best treatment plans, the potential impact of laboratory errors to patient care and safety becomes ever more acute.
The cost of errors in healthcare are reflected not only in terms of direct financial costs to the healthcare system, but also as direct impact on healthcare outcomes. It has been suggested by the Institute of Medicine that up to 98,000 patients die each year in the United States, as a result of preventable medical errors. While this figure has been debated, there is clear acceptance that each year patients are adversely impacted and sometimes die due to medical errors.
With the development and successful implementation of high-quality analytical standards and the automation of the testing process for the majority of common tests, analytical errors are no longer the main factor influencing the reliability and clinical utilization of laboratory diagnostics. Advances in instrument technology, automation and computer science have greatly simplified many aspects of previously tedious tasks in laboratory diagnostics.

THE PRE-ANALYTICAL CHALLENGE
While huge advances have been made within the laboratory to improve the accuracy of laboratory diagnosis and the quality of test results, the pre-analytical process - from the time the test is ordered by the clinician until the sample is ready for analysis – has remained largely untouched. Errors continue to occur and a significant source of these errors can be traced to the pre-analytical process. Pre-analytical errors can account for up to 90% of all laboratory errors. These errors can have a huge impact on the quality patient care, an increased burden and costs to the pathology laboratory, and professional risks for clinicians and the lab.
The challenge for the laboratory is managing and controlling the pre-analytical process which mainly occurs outside of the lab walls and can involve numerous different healthcare practitioners operating at different types of healthcare facilities. While laboratories have implemented procedures to control and detect errors, and in training and certification of their sample collection staff, errors are still occurring due to the fact the pre-analytical process is largely manually managed and reliant on human interventions which are often outside of the control of the laboratory. As the pre-analytical phase involves much more human handling, compared to the analytical and post-analytical phases, pre-analytical errors largely stem from human mistakes. Most pre-analytical errors are preventable.
THE IMPACT
Both detected and undetected errors may cause unnecessary and costly investigations and have consequences for the patient. Further, as there is no automated and systematized approach to error detection there is no guarantee that was the same error to reoccur, that it would be detected next time around.
Pre-analytical errors in the collection of samples for pathology tests can adversely impact patient care, test turn-around times and processing costs for laboratories. With the advances in laboratory instrument technology and the automation of the majority of test procedures, pre-analytical errors are now the source of almost all errors that occur in the testing process. Clearly there is a need to improve the pre-analytical process.
CHASING THE SOURCE OF ERRORS
Electronic ordering and Positive Patient Identification systems can help to reduce errors, but they do not provide the holistic approach that is required to address the scope of pre-analytical errors. To make a dramatic impact to pre-analytical errors an approach is required that can deliver both support and management for each step in the pre-analytical process wherever it may occur, underpinned by an understanding of why errors occur and integrating best practice methods that eliminate errors.
There is currently a barrier for laboratories to effectively control and manage the pre-analytical process. Manual procedures that operate at the laboratory to record errors that occur within the pre-analytical process do not enable the laboratory to effectively monitor of each step of the pre-analytical process as they are being performed outside of the laboratory environment, or to fully analyse the source and causes of errors. As a result, the laboratory becomes reactive to pre-analytical errors – they do not presently have the ability to control and monitor the performance of the steps in the pre-analytical process in “real time”. Therefore, the laboratory’s ability to quickly and effectively identify the source and cause of error is severely impaired.

The pre-analytical process occurs mainly outside of the laboratory walls and generally outside of the control of the laboratory. It predominantly relies on the vigilance and expertise of people at every step, and has remained largely untouched in the evolution of laboratory work practices. To prevent errors the lab needs the ability to deeply analyse the source and determine the cause of errors. With this knowledge, targeted and focused corrective action can be more efficiently directed to the source of the error – for example, a particular procedure, collection staff or specimen transportation method. Collection of the data that supports this type of analysis must be integral with each step as it is performed with sufficient depth to provide the understandings needed. This enables the lab to monitor pre-analytical performance in real time, and direct corrective actions more quickly and efficiently.
Clearly there is a need to improve the pre-analytical process. Much attention has been focused in recent years in the implementation of electronic ordering systems to allow physicians to initiate test orders, however this addresses only part of the pre-analytical process. To make a dramatic impact to pre-analytical errors a holistic approach is required that can deliver both support and management for each step in the pre-analytical process.
FINDING A SOLUTION
While laboratories have implemented procedures to control and detect errors, and in training and certification of their sample collection staff, errors are still occurring due to the fact the pre-analytical process is largely reliant on human interventions. In addition, often much of the pre-analytical process is outside of the control of the laboratory. Orders are generated by doctors at surgeries and hospitals, and samples may be collected externally to the laboratory as part of patient consultations, emergency care or surgery. Human errors will inevitably occur and these errors represent a risk to patient safety and costs to the laboratory and the broader healthcare system.
The pre-analytical process is a broadly distributed process that may involve numerous healthcare workers operating at geographically dispersed locations. Collections can be sourced at clinics, hospitals and ancillary care facilities as well as at patient homes. Test orders can be generated by doctors operating at hospitals, surgeries and clinics. In this environment, transportation of samples between the point of collection and the testing laboratory must also be controlled.

This has made the pre-analytical process disjointed, difficult to control and effectively manage. While attempts have been made to provide technology solutions to areas highly prone to errors (e.g. electronic ordering, Positive Patient Identification), no comprehensive solution has been delivered that enables the pre-analytical process to be measured, monitored and managed.
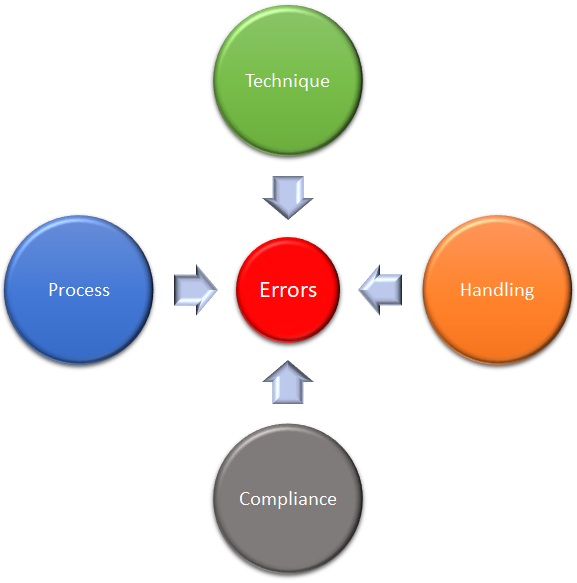
Understanding that errors can be caused through failures in process, technique, handling or compliance means that eliminating pre-analytical errors requires an integrated solution capable of supporting each of these elements at each point in the process. To be most effective, the solution must be inclusive of all healthcare workers and provide point-of-care support regardless of where and when each step is performed. In addition, the solution must be able to be actively managed and measured – providing visibility and control to the laboratory and clinicians. This was the starting point for PAMS.
PAMS delivers the opportunity to not only comprehensively address pre-analytical errors, but to re-engineer the delivery of the pre-analytical process, unifying the relationship between the laboratory, clinicians and patients. Using mobile technology combined with a sophisticated suite of applications that can be tailored to a vast array of collection and management applications, these errors can largely be eliminated.
This dramatic new approach makes elimination of pre-analytical errors a realistic opportunity.
GET THE FACTS
Get our complementatary publication that sets out the facts around how and why pre-analytical errors occur, the impacts of those errors, and how they can be prevented.
Find out how to:
- Eliminate errors
- Reduce recollections
- Improve patient safety
- Improve profits
- Protect your reputation and reduce the risk of litigation
- Efficiently scale-up or down resources to meet fluctuating demands
This free publication examines case studies that demonstrate how PAMS can be used to prevent pre-analytical errors with real ROI and results.